What Do We Know by Richard Jones
This is what we know.
We know that in any given year, only 10% of those with an addiction issue receive any type of assistance or help.
As it currently stands, we are having difficulty meeting the needs of the 10% that do show up. Can you imagine if the other 90% showed up? It would be an absolutely unmanageable situation.
We know we are in need of some serious changes. We know we need real innovation.
What do we know about innovation in general?
When you learn about innovation there are some clear factors that are universal across all industries.
Two of the most pronounced issues associated with innovation are business models and governing beliefs.
Business model is straightforward. It’s the “how we do what we do to make enough money to keep doing what we do”. Governing beliefs can be overtly stated, but many times, these are the unspoken rules and perspectives that drive the industry.
Rotman Management Magazine states that “every industry has it’s governing beliefs”.
These beliefs tend to drive decisions and many times will be a barrier to innovation. According to Rotman no industry is beyond developing dysfunctional governing beliefs.
Let’s explore these factors a little closer:
You cannot innovate within an existing “business model”.
All you can do is incremental improvement. The existing traditions, norms, culture, practices, ingrained thinking will always “rub off” the innovation.
They will take the square peg and shave it down until it fits into a round hole.
For example, the addiction conferences where they talk about an “app” to monitor the behavior of an already engaged and willing client…that’s not innovation. That’s an upgrade.
Like adding remote start to your Toyota Camry. It’s cool. But not innovation. All the fundamentals remain the same.
In all industries the business model is driven by governing beliefs:
Therefore, in order to have innovation we must change governing beliefs. We must have a paradigm shift. The prevailing governing beliefs of addiction treatment/recovery services currently are:
- A person must experience sufficient consequences and “pain” in his life in order to become “willing” to “enter treatment”.
- If the person does not succeed in treatment (or post treatment) it is generally his fault. Mainly: “he wasn’t ready”.
- Multiple trips to rehab and to treatment is good for business. There is no incentive to keep people out of rehab. There is no incentive to support after-care in anything that resembles a substantive way.
- Generally speaking there is one way to recover and it involves completion of treatment followed by attendance to community-based meetings.
- The real money is made in the residential space and the main way we fill beds is either business development staff (the light) and/or SEO ; pay per click; patient brokering; make me throw up marketing strategies (the dark).
Nothing new. Just more convenient.
Innovation, to this point, has taken place within the context of these fundamental beliefs:
An example of this is the explosion of “recovery apps” that pre-suppose “a willing and engaged” participant.
The participant “inputs data” and they tracks their own progress. The participant receives feedback and direction and is receptive to all that.
This app follows the governing beliefs of the industry. Namely, a participant must be actively engaged, motivated and willing to become involved. Nothing new. Just more convenient.
Rehab is the Answer. Why?
Another example can be found in all the “family advocacy/recovery programs” that are primarily focused on “getting people into inpatient treatment”.
They adhere to the governing belief that “rehab is the answer”. Why?
What about the foundations and scholarship funds dedicated only to “beds”. Why?
What about the government over-emphasis on dollars for treatment and the outright disregard for recovery support services. Why?
Does anyone ever take a moment and actually question “Why are we doing it this way”?
Especially in light of the results we are getting!
Every other industry is in a constant state of creative destruction and innovation. The advancement of the human race is built on innovation.
A Complete 180
It stands to reason then, that in order to embrace true innovation, we would need to turn the paradigm 180 degrees:
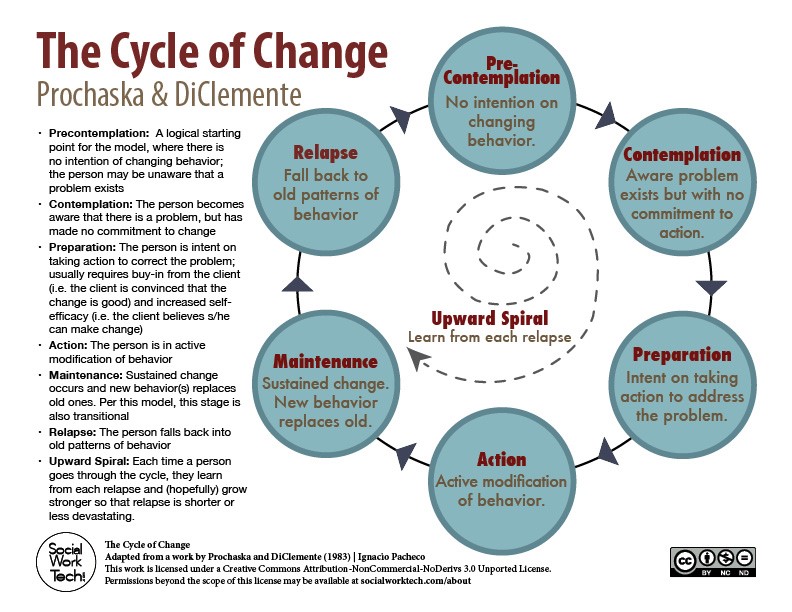
- A person DOES NOT have to “want it” in order to get better. Indeed, most people are not internally motivated when they enter recovery. Waiting for “bottom” is illogical and inhumane.
- A PRIMARY RESPONSIBILITY OF TREATMENT/RECOVERY/HEALTHCARE is to find and engage these people before they get worse.
- If a person does not succeed in treatment (or post treatment) the primary responsibility lays at the feet of the provider (of course there will be exceptions to this rule).
- Providers should make more money if the person is successful post rehab/treatment. Multiple trips to treatment is a sign of a flawed program.
- Invent brand new ways to recover and allow the participant to guide that process.
- Residential treatment should be an afterthought as the real work is done in the community and reimbursement should reflect this reality. A de-emphasis on “filling rehab beds” would be a game changer. We could then spend our time on finding solutions.
The most obvious questions are:
- Why is innovative thinking so rare in the addiction treatment space?
- Why is it so difficult to challenge our governing beliefs?
The simple answer is the PLAYERS, FUNDING AND REGULATIONS makes the treatment industry landscape infertile ground, in terms of much needed innovation.
NOTE: In order to understand the barriers to innovative thinking in addiction treatment we will use macro-level healthcare innovation as a context.
Harvard Business Review
In the article “Why Innovation in Health Care Is So Hard” Harvard Business Review identified 6 “forces” affecting innovation. Let’s will look at some of these areas and see how they apply to addiction treatment.
THE PLAYERS –
As HBR states:
“The health care sector has many stakeholders, each with an agenda. For example, hospitals and doctors sometimes blame technology-driven product innovators for the health care system’s high costs.
Medical specialists wage turf warfare for control of patient services, and insurers battle medical service and technology providers over which treatments and payments are acceptable.
Inpatient hospitals and outpatient care providers vie for patients, while chains and independent organizations spar over market influence.
Nonprofit, for-profit, and publicly funded institutions quarrel over their respective roles and rights. Patient advocates seek influence with policy makers and politicians, who may have a different agenda altogether—namely, seeking fame and public adulation through their decisions or votes”.
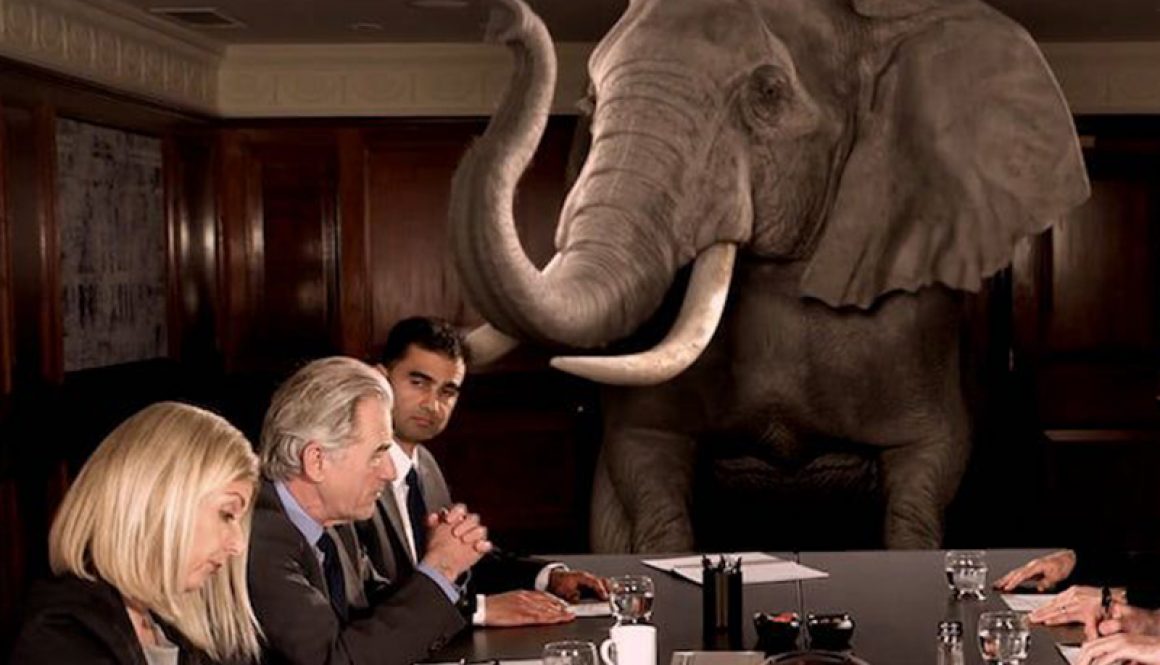
THE HOLY COW!!!
Tell me this doesn’t apply to the addiction treatment and recovery space?
Private treatment providers are in the midst of an unprecedented controversy surrounding ethics. There is ongoing debate about evidence-based treatment. Abstinence based organizations and medication assistance advocates each dig in and establish their righteous positions.
Status quo organizations do not want new programs and new approaches to come on board.
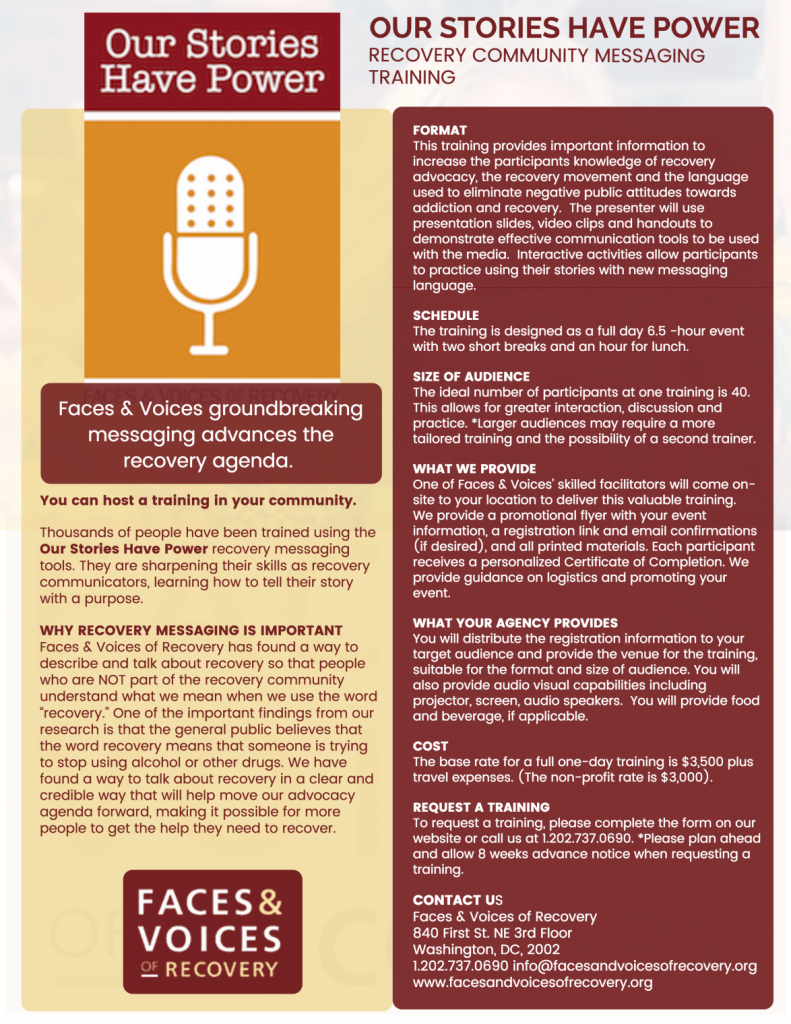
The recovery movement has its own ethical controversies. Pharmaceutical companies are a player, whether we want to admit it or not. There are new advocacy organizations popping up every other day.
Public treatment providers have a lobbyist group that ensures public funding continues to funnel through the Single State Authority.
There are competing interests. Despite the fact most players consistently state there is “no competition”.
These complex and competing interests make innovation very difficult.
If we are going to innovate we are going to need to minimize push back. The effective innovator will need to understand “both sides of the fence” and nurture relationships across these competing domains.
THE FUNDING –
HBR states
“Innovation in health care presents two kinds of financial challenges: funding the innovation’s development and figuring out who will pay how much for the product or service it yields”.
Of course, this is a major barrier to innovation in addiction treatment and recovery services. Insurance companies and government policy makers have defined a relatively narrow scope of “reimbursable” services.
These reimbursement policies drive program development. Providers develop interventions, programs, and solutions. All based on “how they get paid”, rather than, “what’s best for the patient”. Who can blame them?
At its most fundamental level our “fee for service” model “incentivizes” multiple trips to treatment. Rinse and repeat is desirable from a business model standpoint.
A move toward value-based healthcare and reimbursement based on outcomes could go far in promoting true innovation. If we incentivize outcomes over episodes of care we may see new ideas emerge.
THE POLICY –
HBR states:
“Government regulation of health care can sometimes aid innovation (“orphan drug” laws provide incentives to companies that develop treatments for rare diseases) and sometimes hinder it (recent legislation in the United States placed a moratorium on the opening of new specialty hospitals that focus on certain surgical procedures). Thus, it is important for innovators to understand the extensive network of regulations that may affect a particular innovation and how and by whom those rules are enacted, modified, and applied”.
In the addiction treatment and recovery services domain regulation slows innovative and non-traditional services have difficulty in being recognized as legitimate alternatives. These restrictions are frequently tied to funding.
For example, only certain licensed professionals can provide reimbursable services. Recovery coaching services are rarely reimbursed. Services can only be delivered in “licensed clinics”.
The program is restricted to working with the “identified patient”.
These regulations ensure most providers stay within the box. Otherwise you go out of business.
The key is to find alternative funding to implement the innovation. This will give the innovator a chance to demonstrate the effectiveness and value of the innovation which could lead to eventual regulatory approval. This could ultimately lead to reimbursement.
What do we do?
The first step is always awareness and recognition. If we consider ourselves innovators we must recognize these challenges and game-plan accordingly. There is nothing easy about innovation.
We will need to work with all of players to challenge the existing funding and regulations.
But more important than anything.
We will need to come up with the innovative solutions required to meet the needs of 22 million untouched individuals with substance use disorder and 100 million plus overwhelmed family members.
“We have some serious work to do.”- Rich Jones




 NA and People on Medically Assisted Treatment –
NA and People on Medically Assisted Treatment –